In today’s highly regulated world, businesses, especially those in pharmaceuticals, biotechnology, medical devices, food, and software, must prove that their processes work exactly as intended. This proof isn’t optional; it’s the backbone of compliance, quality, patient safety, and long-term trust.
That’s where Validation Services come in.
Validation is more than documentation or technical tests. It’s a disciplined, structured approach to ensuring products, systems, and processes perform reliably every single time. Whether you’re launching a new system, upgrading legacy equipment, or preparing for an FDA audit, validation services protect your organization from costly risks and bring peace of mind that everything is running safely and consistently.
In simple words: Validation Services help you show evidence that what you build, manufacture, test, or automate is actually working and that it can stand up to regulatory scrutiny.
Why Validation Services Matter
For many teams, validation can feel overwhelming. There are documents, audits, protocols, templates, and shifting regulatory expectations. Yet, at its core, the goal is simple:
1. To ensure processes are repeatable
2. To ensure systems are accurate
3. To ensure products are safe
When done right, validation creates confidence—for manufacturers, regulators, employees, and most importantly, customers.
Types of Validation Services
Different industries require different types of validation. Here’s a simplified breakdown to help you understand how they work and where they apply.
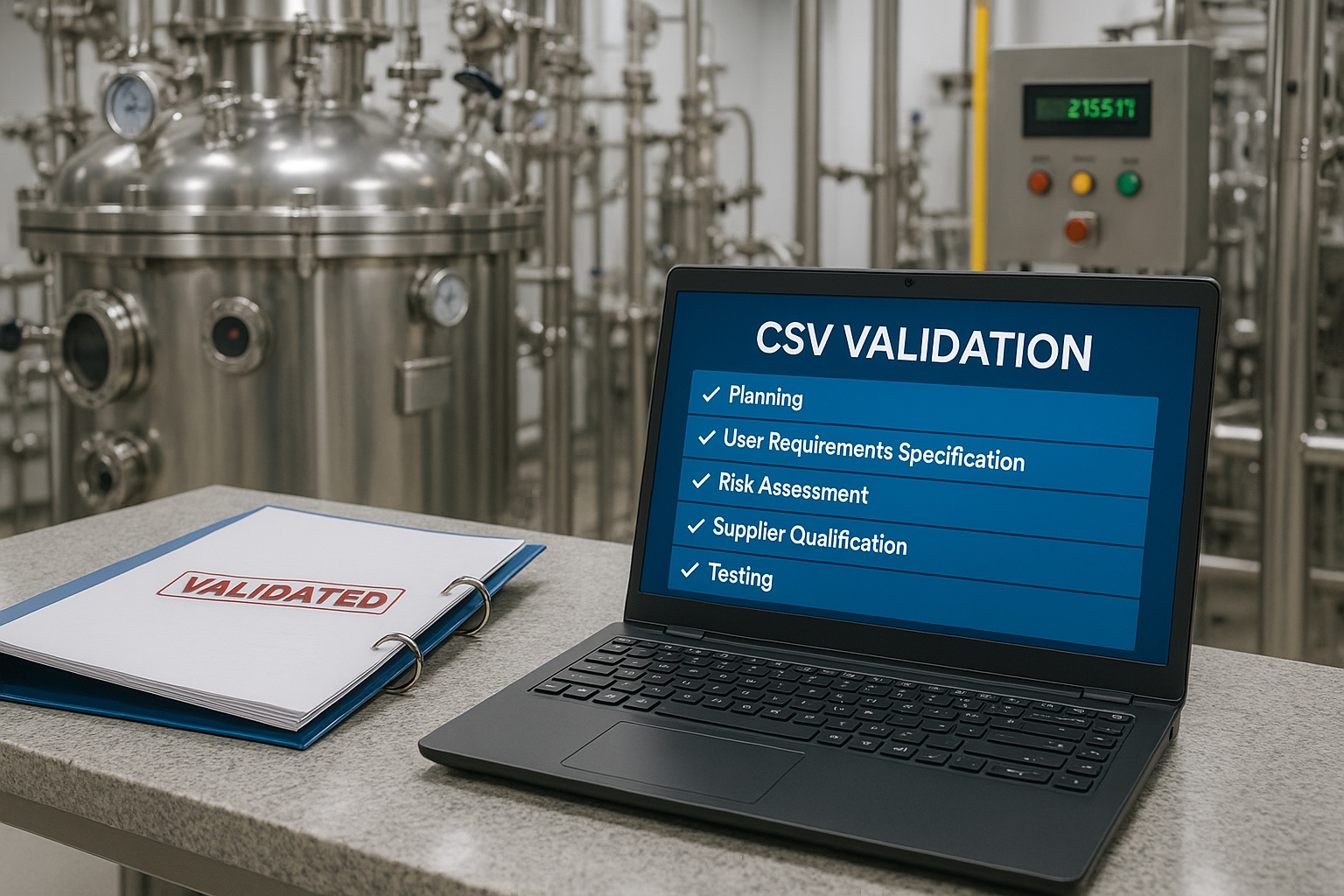
1. Computer System Validation (CSV)
This ensures software and computerized systems used in regulated environments work correctly and consistently.
Used for:
1. Laboratory systems
2. Manufacturing execution systems
3. ERP, LIMS, QMS, CRM
4. HRMS and medical systems
5. Electronic batch records
CSV evaluates whether the system meets user requirements, regulatory expectations (like FDA 21 CFR Part 11), and data-integrity principles.
2. Process Validation
This confirms that a manufacturing process can reliably produce quality products across multiple batches.
Used in:
1. Pharmaceuticals
2. Biologics
3. Medical devices
4. Food manufacturing
Process validation is usually performed in three stages:
- Process Design
- Process Qualification
- Continued Process Verification
3. Equipment Qualification (IQ, OQ, PQ)
This verifies equipment performance through Installation, Operational, and Performance Qualification tests.
Quick Overview Table
| Qualification Stage | What It Checks | Example Activities |
| IQ – Installation Qualification | Was the equipment installed correctly? | Utility checks, component verification |
| OQ – Operational Qualification | Does it work within defined limits? | Functionality tests, alarms, controls |
| PQ – Performance Qualification | Can it perform under real conditions? | Batch runs, performance consistency |
4. Cleaning Validation
Ensures that cleaning procedures remove contaminants, residues, and microorganisms from equipment surfaces.
- Essential for:
1. Pharmaceutical manufacturing
2. Nutraceuticals
3. Sterile products
4. Chemical processing
Cleaning validation protects patients and prevents cross-contamination.
5. Method Validation
Verifies that laboratory testing methods are accurate, precise, specific, repeatable, and robust.
6. Data Integrity Validation
This ensures data is complete, consistent, and accurate from creation to archival.
Focused on ALCOA+ principles:
Attributable, Legible, Contemporaneous, Original, Accurate + Complete, Consistent, Enduring, Available
Why Companies Use Validation Services
Here are the most common reasons organizations rely on professional validation experts:
- Regulatory Compliance
FDA, EMA, MHRA, WHO, and other regulators demand well-validated systems and processes.
- Risk Reduction
Validation minimizes the chances of product failure, recalls, or compliance violations.
- Audit Preparedness
Having proper validation documentation helps you pass audits with confidence.
- Operational Efficiency
Validated processes reduce downtime, errors, and rework.
- Improved Product Quality
Every customer receives a safe, consistent, reliable product.
How Validation Services Usually Work
Here’s a simplified end-to-end flow of how a validation project is executed:
1. User Requirement Specification (URS)
Define what the system or equipment must do.
2. Risk Assessment
Identify what could go wrong and prioritize critical parameters.
3. Validation Plan
Create a roadmap for documentation, testing, and responsibilities.
4. Protocol Development
Prepare IQ, OQ, PQ, CSV protocols, test scripts, templates, etc.
5. Execution
Perform the actual testing and evidence gathering.
6. Deviations & Resolutions
Investigate failures, document root causes, and implement fixes.
7. Final Report
Summarize findings and provide documented proof of validation.
A Simple Comparison Table
| Area | Without Validation | With Validation |
| Compliance | Risk of violations, major audit findings | Smoother audits, clear documentation |
| Product Quality | Inconsistent batches | Predictable quality |
| Operational Stability | Frequent breakdowns or failures | Reliable performance |
| Risk Exposure | High recalls, customer complaints | Minimized risks |
| Trust | Reduced credibility | Higher customer and regulatory trust |
Industries That Rely on Validation Services
Validation is essential across a wide range of fields:
1. Pharmaceuticals & Biotech
2. Medical Devices
3. Food & Beverage
4. Cosmetics
5. Healthcare & Hospitals
6. Software as a Medical Device (SaMD)
7. Laboratories
8. Manufacturing Industries
Whether it’s automated equipment, lab instruments, new machinery, or cloud-based systems, validation ensures everything works exactly as intended.
Key Highlights & Pointers
Here are some quick pointers that make validation easier to understand:
- Validation is not a one-time activity it’s ongoing.
- Documentation is just as important as testing.
- Every validation must be risk-based, not overly complicated.
- Data integrity is a core requirement in all validation projects.
- Automation and advanced digital tools are improving validation timelines.
- A validated system must be maintained, reviewed, and monitored regularly.
A More Human Perspective: Why Validation Matters
Behind every medicine that a patient takes, behind every medical device, behind every safety report or laboratory test—there is a system responsible for that accuracy.
People can get hurt when systems fail.
At the root, validation is the protection of people. It makes sure that every pill, every medical device, every batch, and every dataset has been made with due care, precision, and accountability.
For manufacturers, validation eliminates the guesswork. For auditors, it provides traceability. For employees, it brings confidence. And for customers, it builds trust.
That is why validation services are much more than technical tasks; they are quality guardians.
Conclusion
Validation provides the core of quality assurance in highly regulated industries. Whether one is implementing a new system, scaling up manufacturing, launching a medical device, or preparing for an audit, validation ensures that everything performs consistently and safely.
Whether your organization is seeking stronger compliance, better product quality, or operational efficiencies, engaging the right validation experts can transform the way you do business.